Interstitial cystitis (IC) or Painful Bladder Syndrome (PBS) is a complex chronic pain condition of the bladder. Triggers, severity and treatment options are individual for everyone and it can take a long time to understand and treat your IC properly. I know how difficult managing chronic pain can be and want to share the best 5 people who helped me manage my chronic pain with interstitial cystitis.
1. Urologist
This title refers to a doctor who specializes in studying or treating the function and disorders of the urinary system. They have a range of scans and tests that they perform and will help you officially reach your diagnosis. They also provide prescription medications to manage your IC. There are further treatments a urologist can provide to treat/manage your IC aside from oral medications such as bladder instillations (medication into the bladder), cauterization of ulcers should you have them, steroid injections or nerve stimulation with the use of electrical currents. Luckily for me, oral use of the tricyclic antidepressant called Nortryptyline in a small dose was sufficient to manage my pain when used in combination with natural supplements and lifestyle changes. Nortriptyline has been known to be effective in treating nerve pain as an off-label use, even in conditions like fibromyalgia However, you may require more of what a urologist can offer, so a consult with them may be a step in the right direction. It can take a long time to get in to see a specialist like this. I had been on a waitlist for two years when I reached a breaking point in my mental and physical health I began to call the office regularly and inquire about the wait time and requested to be put on a cancellation list. The secretary of the specialists’ office was quick to tell me that the doctor is very busy and that he has a lot of people who are sicker than me. Though angry and disappointed at these remarks, I continued to respectfully advocate for myself and explain how debilitating my pain was, requesting that they please consider fitting me in soon. Once I started contacting them on a regular basis, something opened up for me. The best thing you can do is consistently advocate for yourself.
“I learned a long time ago the wisest thing I can do is be on my own side, be an advocate for myself and others like me.”
Maya Angelou Tweet
2. Naturopath
Naturopathy is the study of alternative medicine. My naturopath has optimistic and refreshing energy. She is possibly the most helpful person in my journey with IC. A naturopath looks at the body as a whole when determining a treatment approach. It is incredible what patterns you can discover in relation to your concerns when you look closely at your sleeping habits, stress levels, diet, personal hygiene, elimination patterns and many other factors. My naturopath asked me in-depth questions about all of these concepts and more. She took her time and listened carefully to my answers, never looking at the clock or reminding me that she has other patients to see. Based on our troubleshooting questionnaire, she recommended natural supplements and exercises to help improve my life and condition. She sells most of the recommended products right in her office but very kindly told me, “I don’t care where you choose to buy the products, I just care that you get the correct dose.” I truly believe that she cares more about results for her clients than about getting their money. She is exceptional at what she does and I would recommend a naturopath to anyone, for any health concern. I do rely on modern pharmaceuticals and value them- but I recognize that most come with an array of side effects. With natural medicine, side effects are often less severe or nonexistent. I can treat my current problems without creating new ones. Who wouldn’t want that?
3. Other sufferers
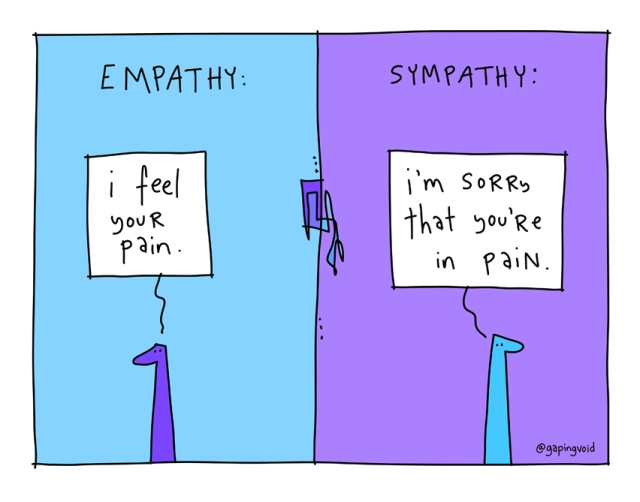
Nobody knows what you’re going through like people who have walked in your shoes. During my desperate search for answers and support, while I waited on lengthy waitlists to see professionals, I joined IC support groups. Facebook in specific has some incredible groups that helped me with recommendations for all of the above treatments (medication, supplements, exercises, food/drink, etc) PLUS immense emotional support. The average person can express sympathy for you, meaning they can acknowledge and maybe even understand your feelings. However, fellow sufferers will express empathy for you, meaning they can actually feel your feelings because they have experienced and lived through them too. Sometimes empathy is what you need to keep pushing in your journey to remission.
4. Gynecologist
A gynecologist is an expert in the female reproductive system. In other words, the vagina doctor. My gynecologist was detrimental in ruling out any other issues. Given my range of symptoms and their location, there are other conditions that can be confused with or mistaken for IC. She provided a thorough examination with a physical and verbal component to rule out other conditions and gave me the peace of mind needed to confidently move forward. She will also be there to guide me on the safety of my IC treatment regime in relation to pregnancy when I am ready for that.
5. Pelvic floor physiotherapist
Physiotherapy is the art of using physical activity and exercises for healing. I am fortunate to have access to a center with physiotherapists that specialize in pelvic floor physio. This is another professional who thoroughly examined me physically and with a lifestyle and symptom questionnaire. She gave feedback on my physical exam after determining that my pelvic floor was hypertonic. A range of exercises was provided to relax the pelvic floor muscles. Though the goal is to remember to do your assigned exercises regularly, even simply being mindful of your muscle tonicity and how it relates to your IC will likely help you, especially in your sex life. We also discussed constipation, something that often contributes to IC pressure and pain given the proximity of the bowel to the bladder. There are exercises to help relieve this too! It is amazing what you can do with simple exercises and mindfulness of how daily activities and body positions affect your symptoms.
I hope that this post gives you some insight into who you can reach out to for support with your interstitial cystitis/painful bladder syndrome journey. This post is specific to IC/PBS but anyone suffering from chronic pain can benefit from discussing their pain with specialists, a naturopath, a physiotherapist and other sufferers of the same condition. Getting the support you need can be challenging at times. I have been where you may be now- having excruciating pain daily and feeling like there is no end in sight- but there are resources out there. Get creative, be persistent and ask around your community for support and recommendations. You can do this. ♡


